Why BPD and Insomnia Make Each Other Worse
Understanding Borderline Personality Disorder (BPD)
Borderline Personality Disorder (BPD) is a severe mental health condition. It affects mood, behavior, and interpersonal relationships. People with BPD experience intense emotions and struggle with self-image and stability.
Core Symptoms of BPD
Common borderline personality disorder symptoms include emotional instability, impulsive behaviors, and fear of abandonment. Many individuals show patterns of idealization and devaluation in relationships. Chronic feelings of emptiness and anger are also frequent.
Emotional Dysregulation in BPD
Emotional dysregulation is a core feature of BPD. Individuals with BPD often react to minor stress with extreme emotional responses. This emotional dysfunction leads to problems in daily activities and sleep.
Paranoia and BPD
Paranoia in BPD tends to appear under stress. This may include intense distrust or fear of being harmed by others. Such symptoms disrupt sleep and worsen mental health.
The Link Between BPD and Sleep Disturbances
Sleep disturbances are common in borderline personality disorder individuals. Many report difficulty falling asleep, staying asleep, or having restful sleep. Subjective sleep complaints align with objective sleep assessments.
Prevalence of Insomnia in BPD Patients
A growing number of studies suggest a high prevalence of insomnia in BPD patients. Chronic insomnia affects both subjective sleep quality and daytime functioning. Compared to healthy control participants, BPD individuals show worse sleep quality and longer sleep onset latency.
Emotional Regulation and Its Role in BPD-Related Insomnia
Poor access to emotion regulation contributes to chronic sleep disturbances. Intense emotions before bedtime increase pre-sleep arousal. Emotional arousal delays sleep time and reduces sleep efficiency.
Impact of Sleep Deprivation on BPD Symptoms
Sleep deprivation amplifies emotional reactivity. This creates a feedback loop, worsening borderline personality disorder traits. Poor sleep quality increases impulsive behaviors and suicidal ideation.
Consequences of BPD and Insomnia Comorbidity
The co-occurrence of BPD and insomnia affects mood, cognition, and health. Research shows that emotional cascades may heighten the risk of self-injury and substance dependence.
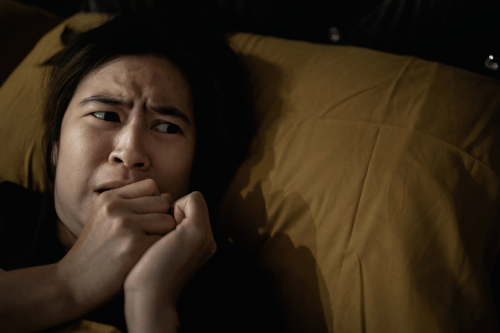
Nightmares and Restless Sleep
Nightmares are common in BPD, often linked to trauma. They contribute to fragmented sleep and higher sleep onset latency. Sleep recordings show increased REM sleep instability in these patients.
Self-Harm and Its Connection to Sleep Patterns
There is a strong link between self-harm and poor sleep. Restless nights lower impulse control and emotion regulation. This makes individuals more vulnerable to emotional cascades and maladaptive behaviors.
Substance Use Disorders Exacerbated by Insomnia
Insomnia in patients with BPD increases the risk for substance use. Some use substances to self-medicate sleep issues. This worsens sleep disorders and emotional dysfunction, creating a harmful cycle.
Mechanisms Underlying the BPD-Insomnia Connection
Several biological and psychological factors explain this connection. These include heightened stress, altered brain function, and maladaptive beliefs about sleep.
Role of Stress and Anxiety
Stress is a key factor in both BPD and insomnia. Increased cortisol and emotional hyperarousal prevent deep sleep. Chronic stress also disrupts circadian rhythms and REM sleep latency.
Neurobiological Factors
Neuroimaging studies show altered activity in the amygdala and prefrontal cortex in BPD. This contributes to difficulties in emotion regulation and sleep onset. Reduced monoamine oxidase activity may also affect mood and sleep.
Cognitive and Behavioral Influences
Cognitive distortions and behavioral habits impact sleep quality. Negative beliefs about sleep and pre-sleep arousal prolong sleep onset latency. Maladaptive sleep cognitions are often seen in BPD individuals.
Therapeutic Strategies for Managing BPD and Insomnia

Evidence-based treatments can reduce both emotional and sleep issues. Dialectical Behavior Therapy (DBT) and Cognitive Behavioral Therapy for Insomnia (CBT-I) show positive outcomes.
Dialectical Behavioral Therapy (DBT)
DBT helps individuals improve emotional regulation and reduce impulsive behaviors. It targets core dimensions like mindfulness, distress tolerance, and interpersonal effectiveness. Clinical predictors suggest that DBT reduces insomnia severity by addressing emotional triggers.
Cognitive Behavioral Therapy for Insomnia (CBT-I)
CBT-I improves sleep efficiency and quality in patients with psychiatric disorders. It focuses on changing sleep-related cognitions and behaviors. Guided internet-based cognitive behavioral therapy also shows promise for treating subjective sleep disturbance.
Integration of DBT and CBT-I
Integrating DBT and CBT-I offers a dual approach. It targets both emotional dysregulation and maladaptive sleep habits. This method addresses the root causes of insomnia in patients with BPD.
Practical Solutions for Better Sleep Management
Along with therapy, practical strategies can help stabilize sleep. Sleep hygiene, mindfulness, and structured routines support emotional and physical health.
Importance of Sleep Hygiene Practices
Sleep hygiene improves time in bed and overall sleep efficiency. Key practices include maintaining a consistent sleep schedule, avoiding caffeine, and reducing screen time. Studies like those by Bastien CH support these behavioral therapies.
Mindfulness Techniques for Enhancing Sleep Quality
Mindfulness lowers emotional arousal and supports better sleep. Techniques include deep breathing and guided imagery. These reduce pre-sleep arousal and improve subjective sleep quality.
Structuring Daily Routines to Support Sleep
Regular routines help regulate circadian rhythms. Scheduling daily activities like meals, light exposure, and exercise can aid sleep continuity. Such routines reduce depressive symptoms and improve quality in patients.
The Role of Professional Help
Professional care is critical for managing comorbid BPD and insomnia. Structured therapy and expert guidance help prevent long-term psychiatric disorders.
Benefits of Structured DBT Skills Groups
DBT skills groups offer peer support and structured learning. They help patients build emotional awareness and self-soothing techniques. Studies by Zanarini MC and Chapman AL show reduced impulsive behaviors and improved sleep time.
Psychotherapeutic Strategies for Managing Insomnia
Therapists can identify clinical variables affecting sleep, such as cognitive control and emotional cascades. Personalized therapy plans help track subjective sleep reports and outcome variables. Clinical interview protocols like the Pittsburgh Sleep Quality Index guide assessment.
Lifestyle Changes for Improving Sleep and Mental Health
Lifestyle changes improve both emotional and physical well-being. These include reducing alcohol use, managing daytime sleepiness, and engaging in regular exercise. Studies in Compr Psychiatry and JAMA Psychiatry link these changes to better sleep efficiency and emotional stability.
Sleep Disorders as Diagnostic and Treatment Factors
Sleep disorders are often overlooked in the diagnosis of borderline personality disorder. However, they significantly affect emotional regulation and clinical outcomes. Diagnostic criteria should consider chronic sleep disturbances as part of the evaluation process for BPD.
The ICD-10 borderline personality disorder classification does not list insomnia as a symptom, but evidence shows it can act as a dependent variable influenced by emotional instability. This insight supports the inclusion of sleep-related symptoms in the clinical assessment of BPD patients. Incorporating sleep data from sleep recordings and subjective sleep measurements provides better diagnostic clarity.
Emotional Instability and REM Sleep Disruption
One major area of focus in BPD and insomnia research is the disruption of REM sleep. Individuals with borderline personality disorder traits often exhibit REM sleep instability and decreased REM latency. This means they enter REM sleep quickly but experience fragmented cycles.
Studies using polysomnographic study methods confirm this instability. These sleep continuity parameters differ significantly from healthy control groups. Emotional arousal and stress hormones likely contribute to this fragmentation, as confirmed by physiological data and subjective sleep reports.
Emotional Arousal and Subjective Sleep Complaints
Heightened emotional arousal before sleep is a consistent predictor of poor sleep quality. This state increases pre-sleep arousal and lowers overall sleep efficiency. Subjective sleep disturbance is often worse than what objective sleep measures reveal, a condition known as paradoxical insomnia.
These subjective sleep experiences are distressing and further impair emotion regulation abilities. Individuals with BPD report greater sleep dissatisfaction even when sleep duration appears within normal ranges. This mismatch between subjective and objective sleep assessments complicates treatment planning.
Cognitive Factors: Maladaptive Sleep Cognitions
Cognitive beliefs about sleep also impact sleep quality in BPD individuals. Maladaptive sleep cognitions—like catastrophizing poor sleep or expecting failure—have been observed in clinical interviews. These negative expectations worsen sleep onset latency and lead to increased daytime sleepiness.
Ociskova M and Prasko J emphasized how such cognitive distortions are more pronounced in patients with emotion regulation difficulties. Treating these beliefs with cognitive behavioral techniques can help shift the mental narrative around sleep. Behavioral therapies targeting these cognitive patterns show promise in clinical trials.
Trauma, Comorbid Depression, and Sleep Quality
Many individuals with BPD have a history of trauma and comorbid depression. These psychiatric disorders independently affect sleep, increasing sleep onset latency and reducing subjective sleep quality. Trauma therapy can address emotional triggers that worsen sleep issues.
In studies by Schredl M and Stuewig J, participants with trauma-related BPD symptoms reported higher levels of subjective sleep complaints. Treating underlying trauma improves not only emotional outcomes but also sleep continuity. Sleep disorders in patients with a trauma background may require integrated treatment plans.
Social Relationships and Sleep Disruption
Interpersonal relationships are another contributing factor to sleep problems. Unstable relationships—one of the core dimensions of BPD—often create emotional distress that lingers into the night. This emotional turmoil contributes to difficulties in emotion regulation and increases sleep onset latency.
Social stress can also elevate cortisol, leading to hyperarousal and fragmented sleep. Supportive environments, or interventions like DBT groups, can reduce social stressors and support better sleep hygiene. Peer support groups also increase compliance with structured sleep routines.
Sleep Issues as Clinical Predictors
Subjective sleep complaints can act as early warning signs of worsening symptoms. Studies have identified poor sleep as a clinical predictor of suicidal ideation and depressive episodes in BPD. Tracking changes in sleep patterns may help therapists predict high-risk periods in patients.
This has important implications for the treatment of insomnia. Tools like the Pittsburgh Sleep Quality Index and daily sleep diaries can measure subjective sleep quality and help identify changes in mental state. Consistent monitoring allows early intervention and reduces hospitalization risk.
Systematic Review Evidence and Research Gaps
A systematic review and meta-analysis of sleep quality in patients with BPD reveals consistent findings: poor sleep efficiency, longer sleep onset latency, and frequent nighttime awakenings. However, more prospective study designs are needed to examine causality.
Most current study protocols use cross-sectional study formats, which provide useful correlation data but lack temporal insight. Longitudinal studies can clarify whether BPD causes insomnia or vice versa. This understanding can influence how behavioral therapy programs are structured.
BPD Sleep Patterns vs. Other Mental Disorders
Sleep in individuals with BPD differs from patterns in depressive disorder or bipolar disorder. While depressed patients may sleep excessively, BPD patients often experience fragmented sleep and shorter duration. Their sleep issues are more associated with emotional arousal than mood stability alone.
Comparing subjective sleep measurements across different mental disorders can clarify symptom-specific interventions. For instance, BPD-specific treatment of insomnia may need a stronger focus on impulse control difficulties and emotional instability than generic depression-focused methods.
The Importance of Sleep Quality in BPD Recovery
Improving sleep quality can enhance treatment outcomes across domains. Better sleep supports cognitive control, reduces emotional reactivity, and strengthens impulse regulation. These factors are critical for managing borderline personality disorder symptoms.
Incorporating sleep as a therapeutic goal in BPD treatment helps patients experience more stability. Improving aspects of sleep like duration, latency, and continuity increases the likelihood of successful long-term recovery. It also reduces reliance on medication or crisis care.
Sleep-Focused Outcomes in DBT Research
Emerging research, including findings from Fitzmaurice GM and Maich KHG, shows that DBT can improve sleep-related outcome variables. Specific modules on mindfulness and distress tolerance have demonstrated positive effects on subjective sleep quality.
This is important because many treatment programs overlook sleep as a target. Integrating structured sleep goals into DBT homework and tracking tools could enhance results. Treat MH Tennessee incorporates sleep-focused goals in our DBT track to address this treatment gap.
Integrating Lifestyle Strategies for Long-Term Change
Lifestyle strategies—like managing light exposure, reducing alcohol use, and exercising—help reinforce treatment gains. These changes are critical in managing symptoms of insomnia and borderline personality disorder long-term. A structured daily routine also supports cognitive control and emotional regulation.
Tracking continuous variables like total time in bed, bedtime consistency, and daytime energy can help therapists assess progress. Combining clinical metrics with lifestyle goals creates a full-spectrum view of the patient’s recovery path.
Final Thoughts
The connection between BPD and insomnia is supported by decades of research, including data from Joiner TE, Perlis M, DeShong HL, and Gunderson JG. From emotional instability to REM sleep disruptions and pre-sleep arousal, the overlap is significant. Sleep quality is more than a secondary concern—it’s a core predictor of BPD stability and functioning.
At Treat MH Tennessee, we treat both emotional dysfunction and sleep issues with a dual-focus approach. We integrate Dialectical Behavior Therapy with modern strategies for managing insomnia, ensuring clients address all aspects of their condition. Our goal is to help individuals not only reduce symptoms but regain a consistent, restorative sleep cycle that supports long-term mental health.
If you’re struggling with sleep issues and borderline personality disorder traits, reach out today. Our evidence-based programs are built to improve your emotional regulation, sleep efficiency, and overall well-being.
FAQ's
Yes, many individuals experience the onset of both conditions during young adulthood, often due to high emotional stress or trauma.
Certain medications can help manage symptoms, but therapy is usually more effective for long-term control of both BPD and sleep issues.
Yes, chronic insomnia may mask or mimic other mental health issues, complicating an accurate BPD diagnosis during clinical interviews.
Improving sleep can reduce emotional reactivity and impulsivity, which may make other forms of BPD treatment more effective over time.