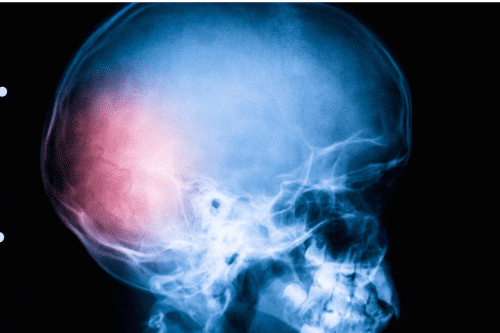
Can Head Trauma Cause Schizophrenia?
Traumatic brain injury (TBI) can trigger lasting changes in brain function, behavior, and mental health. In recent years, researchers have investigated whether TBI can also increase the risk of schizophrenia, a chronic and severe psychiatric disorder. This blog explores current evidence linking head injury to psychotic illness, including studies on family history, genetic risk, and the role of environmental factors in the development of schizophrenia.
Exploring Traumatic Brain Injury (TBI)
Definition and Types of TBI
A traumatic brain injury is brain damage caused by an external force. TBIs are typically categorized as mild head injury, moderate, or severe head injury, depending on the loss of consciousness, memory disruption, and neurological symptoms. Even a mild head injury can lead to long-term psychiatric consequences, especially when repeated or sustained in early life.
Common Causes of TBI
TBIs often occur from motor vehicle accidents, sports collisions, falls, and assaults. Childhood head injury, adolescent head injury, and contact sports are major causes in younger populations. The age at injury, severity of head injury, and age at occurrence are critical factors in determining long-term psychiatric outcomes, including psychotic symptoms, bipolar disorder, and depression after head injury.
Link Between Head Trauma and Mental Health
How TBI May Influence Mental Health Conditions
Trauma to the brain can disrupt neural circuits that regulate emotion, thought, and behavior. This can lead to cognitive symptoms, disruptive symptoms, and even schizophrenia-like psychosis. Brain trauma may result in abnormal neurotransmitter release, inflammation, or axonal injuries—all contributing to changes in mood and perception.
TBIs are linked not only to psychotic disorders but also to substance use disorders, affective disorders, delusional disorders, and behavioral disorders. Studies suggest that the expression of schizophrenia after trauma may relate to both genetic predisposition and epigenetic consequences.
Distinguishing Between Paranoia and Schizophrenia
Paranoia is a symptom that may occur independently or as part of a larger disorder. After a TBI, patients may experience paranoid ideation or hallucinations, but not meet the criteria for schizophrenia. Negative symptoms, such as social withdrawal lack of motivation, and cognitive decline are more specific to schizophrenia diagnosis than to TBI-related psychosis.
Overlapping Symptoms: Paranoia and Hallucinations
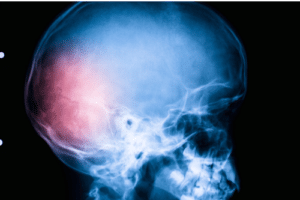
TBI-induced psychosis among individuals exposed to severe brain injuries often includes hallucinations, disorganized speech, and delusional thinking. These symptoms mimic schizophrenia but may resolve over time. Accurate diagnosis depends on medical records, imaging like Magnetic resonance imaging, and understanding the age of onset and history of psychosis.
Understanding Schizophrenia
Definition and Symptoms of Schizophrenia
Schizophrenia is a psychotic disorder characterized by hallucinations, delusions, disorganized thinking, and negative symptoms. It may include cognitive symptoms such as impaired attention and executive function. The onset of psychosis typically occurs in adolescence or early adulthood, but the risk is influenced by many factors for schizophrenia, including environmental medicine, genetics, and traumatic events.
Known Causes and Risk Factors
The risk for schizophrenia increases with family history, particularly in schizophrenia in multiply affected or bipolar disorder pedigrees. Environmental influences, such as urban living, prenatal infections, or early trauma, also play a role. The interaction between head injury and genetic risk may amplify the likelihood of psychiatric illness. Longitudinal birth cohort studies and family studies provide strong support for these links.
Traumatic Brain Injury and Schizophrenia Development
Potential Mechanisms Linking TBI to Schizophrenia
Brain injury can cause structural damage to the frontal and temporal lobes, regions involved in regulating thoughts and behaviors. These changes may lead to psychotic symptoms, including delusional disorder and schizophrenia-like psychosis. Cerebral trauma is believed to contribute to a dose-response relationship, where the severity of head injury directly correlates to the risk of schizophrenia following the trauma.
Damage from axonal injuries, inflammatory responses, and neurochemical imbalances are all potential causes of psychiatric outcomes after a traumatic injury. In some patients, these effects persist, increasing their risk of psychosis following injury.
Case Studies and Research Findings
A chart-based descriptive and case-control study published in the American Journal of Psychiatry highlighted an increase in schizophrenia diagnoses among patients with prior TBI. A 5-year follow-up study confirmed these results, especially when trauma occurred during brain development. Other case-controlled population-based studies and cohort study models found that injury in children and adolescents head injury significantly raised the risk of later psychiatric disorders.
Researchers like Bassett AS, Mors O, and Weissman M. documented a consistent pattern of TBI-related psychosis across diverse populations. Findings from Aalberg V., Blehar MC, Kramer R, and Cathcart S. support a direct association between head injuries and the subsequent development of schizophreniform disorder and affective disorders.
The Role of Genetics and the Environment
Evidence supports a combined risk model, where both genetic risk and environmental exposures like TBI contribute to the development of schizophrenia. Studies also suggest epigenetic consequences of trauma, altering how genes involved in psychiatric illness are expressed. A systematic review in Psychol Med and work by Conroy RM and Cotter DR found that individuals with TBI and a family history of mental illness are at the greatest risk.
Comparing TBI-Induced Conditions to Schizophrenia
Differentiating TBI-Related Symptoms
Schizophrenia-like psychosis following TBI is sometimes called TBI-related psychosis or organic psychosis. These conditions may include hallucinations and paranoia but typically lack the negative symptoms and social decline seen in schizophrenia. Clinicians use imaging tools like Magnetic resonance imaging and voxel-based morphometry studies to assess brain trauma.
TBI and Other Mental Health Disorders
TBI increases the risk for a broad range of disorders, not just psychotic illnesses. This includes bipolar disorder, depression, anxiety disorders, behavioral disorders, and schizophreniform disorder. According to Curr Opin Psychiatry, these risks vary depending on age injury, severity, and environmental factors. Previous studies have found an increased risk of depression, attention in patients post-TBI, and poor quality of life among those affected.
Treatment and Management Options
Psychological and Therapeutic Approaches
Cognitive Behavioral Therapy (CBT) and trauma-informed psychotherapy are effective in treating TBI-related symptoms. These therapies target paranoia, mood disturbances, and cognitive symptoms. At Treat Mental Health Tennessee, we provide specialized care for individuals experiencing psychiatric consequences from traumatic injury, including schizophrenia-like psychosis.
Pharmacological Interventions
Antipsychotic medications may be used in cases of severe psychosis among patients with TBI. Medication plans are tailored based on the history of schizophrenia, previous reviews of side effects, and co-occurring conditions. Environmental medicine practices may also support recovery by addressing physical health, nutrition, and sleep regulation.
Support Systems and Rehabilitation Programs
TBI recovery often requires coordinated care involving psychologists, psychiatrists, neurologists, and caregivers. Treat Mental Health Tennessee offers outpatient and partial hospitalization programs that support recovery from both psychotic disorder and cognitive decline. Rehabilitation focuses on improving attention in patients, restoring function, and building coping skills.
Supporting Individuals with TBI-Induced Paranoia
Strategies for Managing Paranoia
Management begins with education about symptoms and their triggers. Patients benefit from structured environments, daily routines, and low-stimulation settings. Techniques such as mindfulness, journaling, and social support can reduce disruptive symptoms and improve emotional regulation.
The Role of Caregivers and Healthcare Professionals
Caregivers are essential in monitoring behavioral changes and medication side effects. Professionals must consider factors for schizophrenia such as genetic vulnerability, age at onset, and severity of injury. Timely assessment can help distinguish between mental disorders caused by TBI and early schizophrenia expression.
Conclusion: Assessing the Risk
Summary of Findings
Evidence from cohort study models, longitudinal birth cohort research, and case-control studies suggest a meaningful link between TBI and the risk of schizophrenia. The relationship between the severity of trauma and psychiatric illness shows a dose-response relationship, especially when combined with genetic risk or family history. The risk is further influenced by environmental influences, age of occurrence, and adjustment for birth conditions.
Future Research Directions
Ongoing studies using Magnetic resonance imaging, voxel-based morphometry, and genetic screening will clarify how traumatic brain injury contributes to the onset of psychosis. Future critical review papers may expand on the combined risk of schizophrenia in TBI patients with bipolar disorder or other mental illness histories.
Implications for Healthcare and Public Awareness
Clinicians must evaluate the assessment of head injury in psychiatric evaluations and understand how age at injury, severity, and history of psychosis interact. Raising awareness among healthcare providers and families can promote early intervention, potentially lowering the risk for schizophrenia following TBI.
If you or someone you know has experienced brain injury and is showing signs of schizophrenia symptoms, Treat Mental Health Tennessee is here to help. We specialize in treating mental disorders with an evidence-based and individualized approach. Contact us to schedule an evaluation and begin a path toward recovery.
FAQ's
Yes, even mild head injuries like concussions have been associated with a small increase in the risk of developing psychotic symptoms later in life.
Symptoms can emerge months or even years later, depending on age, injury severity, and genetic vulnerability.
Early medical and psychological treatment may lower the risk by addressing neuroinflammation and emotional trauma early.
Yes, cumulative TBIs significantly raise the risk of depression, anxiety, and schizophrenia-like symptoms.